What Can Cause Pain Under The Heel
Overview
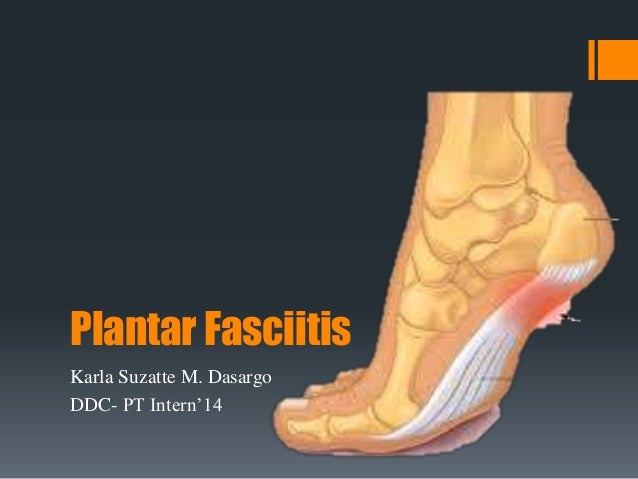
Plantar fasciitis is an inflammation of the structures (of the plantar fascia) on the sole of the foot. The inflammation is caused by excess pressure on the structures on the sole of the foot. The plantar fascia becomes inflamed and tiny rips can occur where it attaches into the inside of the heel bone. It tends to be most painful first thing in the morning, or when standing up after sitting for a while. The area becomes inflamed and swollen, and it is the increase in fluid to the area that accumulates when weight is taken off the area, that then causes the pain on standing. Plantar Fasciitis usually starts gradually with pain on standing after rest. Pain is usually located under the heel or to the inside of the heel. Pain is usually at its worst on standing first thing in the morning. The pain will begin to ease once you get moving. Pain in the early stages tends to occur after activity rather than during activity. As plantar fasciitis continues the pain can become more constant and can then start to affect the way you walk.
Causes
This is a problem of either extreme, so people with high arches or those that have very flat feet are at risk of developing pain in this region. This is because of the relative stress the plantar fascia is put under. In people with excessive pronation, the plantar fascia is put under too much stretch, as their range flattens and strains it. People with a stiff, supinated (high-arched) foot lack the flexibility to appropriately shock absorb, so this too puts extra strain on the plantar fascia. Clinically, we see more people presenting with plantar fascia pain who have excessive pronation than those with stiff, supinated feet. But while the foot type is the biggest risk factor for plantar fasciitis, the whole leg from the pelvis down can affect how the foot hits the ground. A thorough biomechanical assessment will determine where in the kinetic chain things have gone wrong to cause the overload.
Symptoms
Most people with plantar fasciitis have pain when they take their first steps after they get out of bed or sit for a long time. You may have less stiffness and pain after you take a few steps. But your foot may hurt more as the day goes on. It may hurt the most when you climb stairs or after you stand for a long time. If you have foot pain at night, you may have a different problem, such as arthritis , or a nerve problem such as tarsal tunnel syndrome.
Diagnosis
Plantar fasciosis is confirmed if firm thumb pressure applied to the calcaneus when the foot is dorsiflexed elicits pain. Fascial pain along the plantar medial border of the fascia may also be present. If findings are equivocal, demonstration of a heel spur on x-ray may support the diagnosis; however, absence does not rule out the diagnosis, and visible spurs are not generally the cause of symptoms. Also, infrequently, calcaneal spurs appear ill defined on x-ray, exhibiting fluffy new bone formation, suggesting spondyloarthropathy (eg, ankylosing spondylitis, reactive arthritis. If an acute fascial tear is suspected, MRI is done.
Non Surgical Treatment
Plantar fasciitis treatment can be conservative (non-surgical) or invasive (surgical). Among the non-surgical ways to manage plantar fasciitis involves stretching and icing exercises. A night splint which help stretch the Achilles tendon and plantar fascia overnight, so that they can be more easily stretched during the morning. Orthotics that can be custom-made for the feet can also distribute tension on the feet more consistently. Corticosteroid is injected into the affected area to relieve pain and decrease inflammation. Doctors may also use extracorporeal shockwave therapy before considering plantar fasciitis surgery. During the therapy, sound waves are used to stimulate the affected area and eventually heal it. Physical therapy incorporation, deep massage stretching, and other modalities can at times be a helpful adjunct treatment. Surgery for plantar fasciitis is only considered when all other conservative treatments have failed.

Surgical Treatment
In very rare cases plantar fascia surgery is suggested, as a last resort. In this case the surgeon makes an incision into the ligament, partially cutting the plantar fascia to release it. If a heel spur is present, the surgeon will remove it. Plantar Fasciitis surgery should always be considered the last resort when all the conventional treatment methods have failed to succeed. Endoscopic plantar fasciotomy (EPF) is a form of surgery whereby two incisions are made around the heel and the ligament is being detached from the heel bone allowing the new ligament to develop in the same place. In some cases the surgeon may decide to remove the heel spur itself, if present. Just like any type of surgery, Plantar Fascia surgery comes with certain risks and side effects. For example, the arch of the foot may drop and become weak. Wearing an arch support after surgery is therefore recommended. Heel spur surgeries may also do some damage to veins and arteries of your foot that allow blood supply in the area. This will increase the time of recovery.
Stretching Exercises
In one exercise, you lean forward against a wall with one knee straight and heel on the ground. Your other knee is bent. Your heel cord and foot arch stretch as you lean. Hold for 10 seconds, relax and straighten up. Repeat 20 times for each sore heel. It is important to keep the knee fully extended on the side being stretched. In another exercise, you lean forward onto a countertop, spreading your feet apart with one foot in front of the other. Flex your knees and squat down, keeping your heels on the ground as long as possible. Your heel cords and foot arches will stretch as the heels come up in the stretch. Hold for 10 seconds, relax and straighten up. Repeat 20 times. About 90 percent of people with plantar fasciitis improve significantly after two months of initial treatment. You may be advised to use shoes with shock-absorbing soles or fitted with an off-the-shelf shoe insert device like a rubber heel pad. Your foot may be taped into a specific position. If your plantar fasciitis continues after a few months of conservative treatment, your doctor may inject your heel with steroidal anti-inflammatory medication. If you still have symptoms, you may need to wear a walking cast for two to three weeks or a positional splint when you sleep. In a few cases, surgery is needed for chronically contracted tissue.